Excerpted from C. Diff In 30 Minutes: A Guide To Clostridium Difficile For Patients And Families, by C. diff expert Dr. J. Thomas Lamont, M.D.
 Although it may seem unlikely, the stool in your colon serves a very important function. That’s right, the smelly stuff you flush down the toilet is actually extremely important to your overall health and well-being. Your colon (highlighted in the inset image) is loaded with trillions of microorganisms, including bacteria, viruses, and fungi, which live there in perfect harmony with each other and with you. In fact, these tiny organisms count on you to feed and water them every day, just like your pet cat or dog.
Although it may seem unlikely, the stool in your colon serves a very important function. That’s right, the smelly stuff you flush down the toilet is actually extremely important to your overall health and well-being. Your colon (highlighted in the inset image) is loaded with trillions of microorganisms, including bacteria, viruses, and fungi, which live there in perfect harmony with each other and with you. In fact, these tiny organisms count on you to feed and water them every day, just like your pet cat or dog.
About 90% of the food you eat is absorbed by your intestinal tract. Every cell in your body, from the hair on your head to the skin on the soles of your feet, is made from the food you eat.
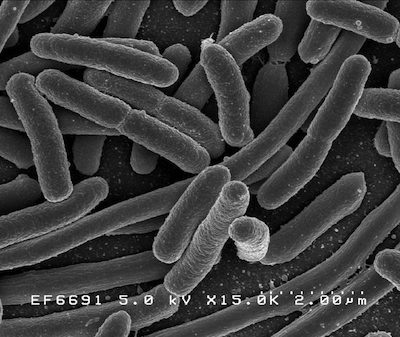
What about the rest? The 10% that’s not absorbed feeds the trillions of bowel flora living in your colon. Ten percent of your diet is mostly plant fibers, cereals, and starches, sometimes called roughage, which cannot be digested and absorbed by humans. For centuries, scientists had little knowledge about the colonic flora, but now it’s clear that the organisms in our stools protect us from invaders like C. diff and other causes of bowel infection. These bacteria in the colon are sometimes called “the barrier flora” because they provide a protective shield against harmful organisms. The image below shows a type of barrier flora, magnified by an electron microscope.
Antibiotics can have a negative impact on the flora in your colon. While antibiotics are used to treat bacterial infections, such as strep throat or tuberculosis, they can also take out the barrier flora and other normal bacteria in your colon.
So, to get C. diff, the first thing that has to happen is that your barrier flora are killed off or weakened by an antibiotic. Once this happens, C. diff can jump in. Clearly this doesn’t happen to everyone who takes an antibiotic. Only about 1 in 100 or 1 in 1,000 people who take an antibiotic will get C. diff. Not all antibiotics are equal in their ability to allow C. diff. Clindamycin, ciprofloxacin, penicillins and cephalosporins are the main offenders, while azithromycin, tetracycline and bactrim are less likely to cause this problem.
The bottom line: Any antibiotic can weaken your barrier flora in the bowel that normally protects you from invasion by C. diff.
To learn more about Clostridium difficile symptoms and treatments, read C. Diff In 30 Minutes: A Guide To Clostridium Difficile For Patients And Families, by C. diff expert Dr. J. Thomas Lamont, M.D.