The following C. diff case study was excerpted from C. Diff In 30 Minutes: A guide to Clostridium difficile for patients and families by Dr. J. Thomas Lamont, M.D.
Al was a very healthy 62-year-old electrician. That is, until he developed an abscess on his wisdom tooth. His dentist prescribed the antibiotic clindamycin for seven days to treat the abscess and scheduled a root canal.
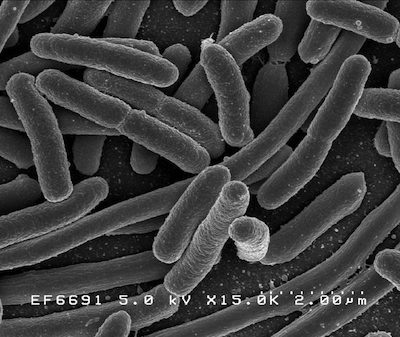
 Five days after Al finished the clindamycin, he developed diarrhea, an upset stomach, and pain in the lower abdomen. The diarrhea was severe, occurring up to 10 times per day. He called his doctor who tested his stools for C. diff. The result was positive. Treatment was started with 10 days of Flagyl (one of the same antibiotics taken by Jeannie) four times per day. By the fifth day, his diarrhea was almost gone and Al was ready to go back to work.
Five days after Al finished the clindamycin, he developed diarrhea, an upset stomach, and pain in the lower abdomen. The diarrhea was severe, occurring up to 10 times per day. He called his doctor who tested his stools for C. diff. The result was positive. Treatment was started with 10 days of Flagyl (one of the same antibiotics taken by Jeannie) four times per day. By the fifth day, his diarrhea was almost gone and Al was ready to go back to work.
Four days later the diarrhea returned. It was as bad as it had been in the beginning. This time, Al’s doctor started him on Vanco (the other antibiotic taken by Jeannie) four times per day. Again, Al appeared to recover, and the diarrhea went away. But eight days after Al stopped the Vanco, it came back — the same smelly diarrhea with lots of mucus and cramps. Al was frustrated now and worried that he might never get rid of his C. diff.
His primary care doctor was frustrated, too. He arranged for Al to see an infectious disease specialist at a teaching hospital in Boston. The specialist recommended a pulse-taper of vancomycin for eight weeks, during which the Vanco was taken in a gradually decreasing dose. It started with one capsule four times per day, and ended with one capsule every other day for the last week.
Al finished the eight weeks of Vanco and followed this up with four weeks of Culturelle, a probiotic. Probiotics are dried bacteria or yeasts that are designed to help the colonic flora, the bacteria and other microorganisms that live in our large bowel (colon), to return to their original state before the patient took antibiotic treatment.
This time, the diarrhea came back two weeks after he stopped taking Vanco. Al’s frustration level went through the roof. He felt that C. diff had taken over his life and he would never get better. He even worried that his C. diff infection was going to be fatal. At that point, his son went online to see what options were available for patients with multiple recurrences of C. diff. He read that many patients like his father got better after a stool transplant.
What is a stool transplant?
Getting a stool transplant is like reseeding a lawn that has been damaged by weeds, drought, and poor soil. The soil is prepared, watered, and seeded, and eventually a new lawn replaces the old. In a stool transplant, the “seeds” are a suspension or “shake” of healthy stool, taken from a healthy donor, and transferred via a medical device to the colon of a person suffering from C. diff. The procedure is straightforward and has a permanent cure rate of 95% among C. diff patients. Chapter 3 describes the procedure in more detail.
Al was eventually referred to a gastroenterologist (GI) specialist at our hospital who had experience with stool transplants to treat C. diff. The doctor explained that the C. diff infection kept coming back because Al’s colonic flora was depleted from all the antibiotics taken over the past three months. The normal colonic flora provides a protective barrier against C. diff, other harmful bacteria, and viruses. That’s why nearly every patient who gets C. diff has taken an antibiotic before the diarrhea starts. But Al’s barrier was so low that the C. diff kept coming back after he stopped the Vanco.
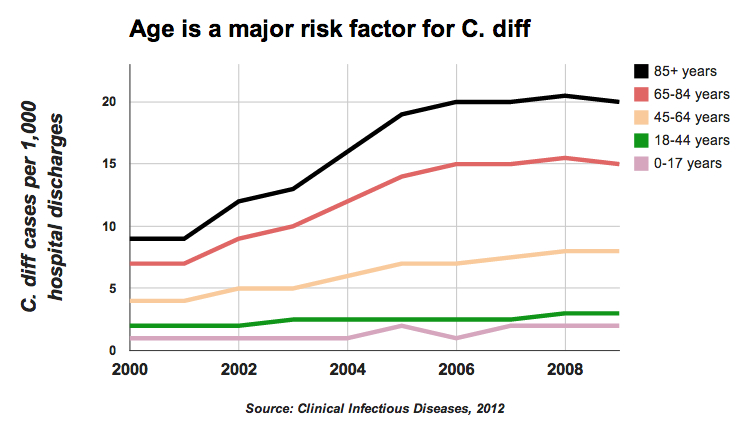
Once patients have had one recurrence, the odds go way up that they will have multiple repeat attacks. We have seen patients with more than 10 such recurrences. They are typically elderly with other illnesses such as heart failure, cancer, or chronic kidney disease, all of which can depress the immune system. Depression, fatigue, and weight loss are very common in so-called “repeaters.”
In order to try a stool transplant, a donor was needed. Al’s wife was healthy, with no diarrhea and no recent antibiotics. The plan was for her to come in with Al on the day of his colonoscopy, and to “donate” a stool sample that would be used to reseed his colon. Her stool was put in a blender with water to make a thin liquid shake, which was then filtered to remove any solid material. The GI doctor then passed a colonoscope to the upper part of Al’s colon and injected some of his wife’s liquefied stool through the scope. Then he slowly withdrew the scope, infusing some of the liquid every four or five inches until he reached the bottom of the colon. Al was instructed to lie quietly for an hour in the recovery area, and then he was discharged home with instructions to take no more vancomycin.
After the transplant Al felt fine. Naturally, he worried that C. diff might come back. When he saw the gastrointestinal doctor three weeks later, he had no diarrhea, the longest time he had been without symptoms since the root canal. Three months after the stool transplant, Al was feeling great and working full time. He was cured!
At our hospital we have performed dozens of stool transplants for patients with recurrent C. diff. All but one were completely successful, and the one patient who failed had a second attempt that was eventually successful.
For C. diff patients who have tried everything, stool transplants can make a huge difference. Some patients are afraid to try a stool transplant because it seems “gross” or “yucky.” But in hundreds if not thousands of patients worldwide the procedure is safe and very effective. The source of the stool is usually a family member or friend. For a lot of our patients who have recurring C. diff, the choice is either a transplant or more antibiotics for a long time.
To read additional C. diff case studies, download or purchase our C. diff book.

 Fecal microbial transplant (FMT), also known as stool transfer or stool transplant or fecal transplant, is a revolutionary treatment for C. diff patients that is constantly evolving. While the treatment at one time required a colonoscopy, there are now other options. In the following interview, C. Diff In 30 Minutes author and Harvard Medical School Professor J. Thomas Lamont discusses new FMT stool transfer methods.
Fecal microbial transplant (FMT), also known as stool transfer or stool transplant or fecal transplant, is a revolutionary treatment for C. diff patients that is constantly evolving. While the treatment at one time required a colonoscopy, there are now other options. In the following interview, C. Diff In 30 Minutes author and Harvard Medical School Professor J. Thomas Lamont discusses new FMT stool transfer methods.
 In January 2020, J. Thomas Lamont, M.D. (author of
In January 2020, J. Thomas Lamont, M.D. (author of 

 Five days after Al finished the clindamycin, he developed diarrhea, an upset stomach, and pain in the lower abdomen. The diarrhea was severe, occurring up to 10 times per day. He called his doctor who tested his stools for C. diff. The result was positive. Treatment was started with 10 days of Flagyl (one of the same antibiotics taken by Jeannie) four times per day. By the fifth day, his diarrhea was almost gone and Al was ready to go back to work.
Five days after Al finished the clindamycin, he developed diarrhea, an upset stomach, and pain in the lower abdomen. The diarrhea was severe, occurring up to 10 times per day. He called his doctor who tested his stools for C. diff. The result was positive. Treatment was started with 10 days of Flagyl (one of the same antibiotics taken by Jeannie) four times per day. By the fifth day, his diarrhea was almost gone and Al was ready to go back to work.